Loneliness and Social Isolation As Social Determinants of Health
Social isolation and loneliness, often neglected, can have a significant impact on patients’ overall well-being, especially for elderly patients.
According to the Centers for Disease Control and Prevention (CDC), loneliness and isolation may be shaped by many factors, including culture, demographics, and the places where people live, work, learn, and play. Common factors that lead to social isolation and loneliness include long-term illness or disability, domestic violence, loss of a loved one, moving to a new place, migration, aging, and homelessness.
Research suggests that loneliness impacts some groups more than others, including:
- Low-income adults
- Young adults
- Older adults
- Adults living alone
- People with chronic diseases and disabilities
- Immigrants
- Individuals who identify as lesbian, gay, bisexual, transgender, and questioning (or queer)
The Effects of Loneliness and Isolation on Health
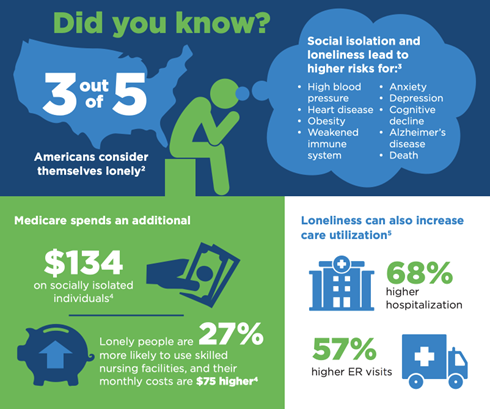
Social isolation and loneliness have serious health consequences. Their health risks are comparable to smoking daily, excessive drinking, and obesity. They can lead to higher risks for:
- High blood pressure
- Heart disease
- Obesity
- Weakened immune system
- Anxiety
- Depression
- Cognitive decline
- Alzheimer’s disease
- Early death
- Dementia
In contrast, high-quality and meaningful social connections are essential to mental and physical health. High levels of social support can positively influence health outcomes through behavioral and psychological pathways. For example, social support may help people stick to healthier diets and reduce emotional stress. According to research, strong social connections and networks can boost a person’s lifespan by 50%.
Did you know?
- More than half of U.S. adults (58%) are considered lonely
- Medicare spends an additional $134 monthly on each socially isolated individual
- Lonely people are 27% more likely to use skilled nursing facilities, and their monthly costs are $75 higher
- Loneliness can also increase care utilization
- 68% higher hospitalization
- 57% higher ER visits
How Can You Help as a Physician?
1. Start the conversation with patients on loneliness and isolation
Create space for patients to talk about their loneliness. Use validated screening tools and questions to assess patients' emotional well-being. Resources like the UCLA Loneliness Scale can guide these conversations and assess how patients are feeling.
2. Encourage patients to build meaningful connections
Share the 24/7 Institute on Aging’s Friendship Line for people 60+ experiencing mental health challenges or loneliness: 1 (888) 670-1360. You can also suggest prayer lines or pen pal programs.
3. Know the local resources and share them with your patients
Provide a list of local services such as adult day care centers, support groups, and volunteer opportunities like foster grandparent programs. These resources can be found through community directories or local health departments.
4. Assure your patients that they’re not alone
Remind patients they can call 211 to connect with human service agencies and community organizations that can best help those in need of assistance. Additionally, share relevant mental health resources from the World Health Organization (WHO).
5. Identify patients at risk and offer timely support
If a patient seems to need more urgent help, share the 24/7 National Suicide Prevention Lifeline for people in emotional distress or suicidal crisis who need support: 988.
Conclusion
Older adults often find themselves spending more time alone, leaving them more vulnerable to loneliness and social isolation. Physicians should pay attention to the signs of these symptoms and provide the resources to help patients build meaningful connections that will improve their physical and mental health.
To read more insights on our “Breaking Down Barriers” series, check out the CareAllies resources page.