Violence as a Social Determinant of Health
According to the World Health Organization (WHO), violence is a major public health problem and a social determinant of health. Violence and abuse can have both physical and psychological impacts on a patient’s well-being. As cited by Healthy People 2030, types of violence include but are not limited to child abuse and neglect, firearm violence, intimate partner violence, sexual violence, and elder abuse. While violence and abuse can affect anyone of any age, certain groups of people are more likely to be exposed. This includes women, the elderly, black adolescents, and young adults, as well as those from low-income communities.
How Does Violence as a Public Health Issue Affect a Patient’s Well-Being?
Violence affects billions of peoples’ lives each year physically, through death, injury, and detrimental impacts on neurological, cardiovascular, immune, and other biological systems. It can also have long-term emotional effects, such as depression, mental health disorders, anxiety, and more. In addition, violence not only affects the victims themselves, but also their families, friends, neighbors and communities as a whole.
Did you know?
- 4.4M people globally lose their lives to violence each year
- Interpersonal violence increases susceptibility to emotional, behavioral, and physical health problems
- 1 out of 4 men and 1 out of 3 women have been in abusive relationships
- Survivors of elder abuse have higher rates of depression, hospitalization, and institutionalization. They are also 3 times more likely to die prematurely
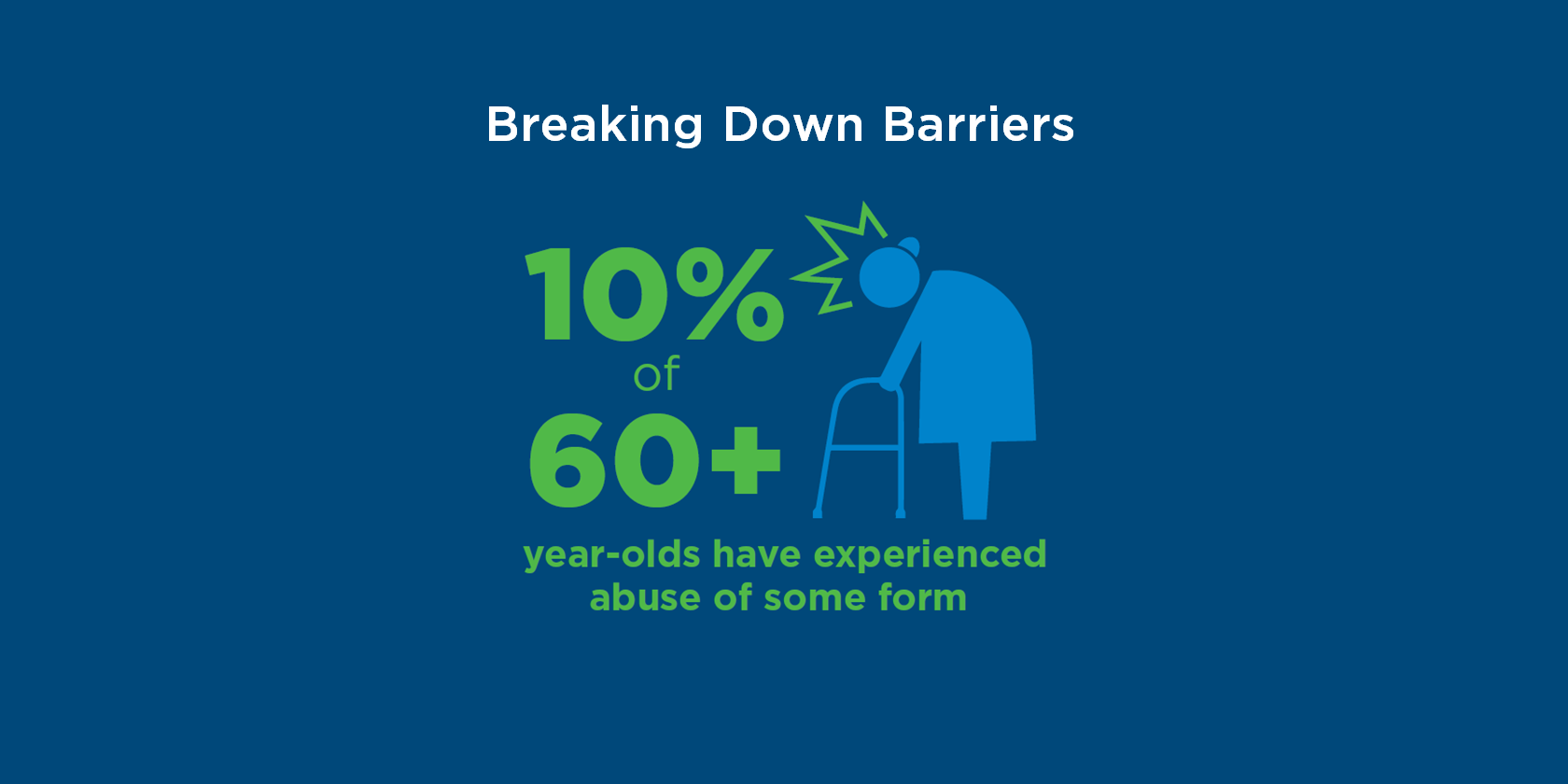
- 10% of 60+ year-olds have experienced abuse of some form
- Low social support increases the risk of all forms of elder abuse
- Nearly 50% of dementia patients experience some type of abuse

How Can You Help as a Physician?
1. Learn about different types of violence and know the facts
Take time to understand how violence can impact patients of all ages.
2. Communicate with patients to proactively recognize signs of violence
Physicians can help mitigate an abusive situation by talking with patients openly. Learn the red flags of abuse and how and when to report it. Educate patients and facilitate their awareness of when someone is harming them. The American Academy of Family Physicians (AAFP) has cited a US Preventive Services Task Force (USPSTF) recommendation for screening women of reproductive age and older or vulnerable adults for intimate partner violence.
3. Be an advocate in preventing violence and abuse
Get involved in elder abuse prevention efforts through the National Center on Elder Abuse. Physicians can learn more about communicating with patients through Talking Elder Abuse.
4. Provide patients with local resources for help
Get familiar with local resources available and connect patients with national resource centers. If there’s a reasonable suspicion that abuse or neglect regarding a patient has been or is being committed, you can contact the authority referenced by NCEA.
5. Share the knowledge and encourage community involvement
Educate others by sharing 12 things everyone can do to help prevent elder abuse. Encourage both medical professionals and patients to engage in community-based efforts.
Conclusion
Overall, recognizing violence as a social determinant of health is important for health care professionals. By understanding the forms and impacts of violence and abuse, physicians can better help mitigate its effects on patients’ well-being and foster healthier communities.
To read more insights on our “Breaking Down Barriers” series, check out the CareAllies resources page.