For security reasons, Cigna.com no longer supports your browser version. Please update your browser, or use an alternative browser such as Google Chrome, Microsoft Edge, or Mozilla Firefox for the best Cigna.com experience.
Accountable Care Is Here To Stay
Corey Redding – Vice President, Direct Contracting
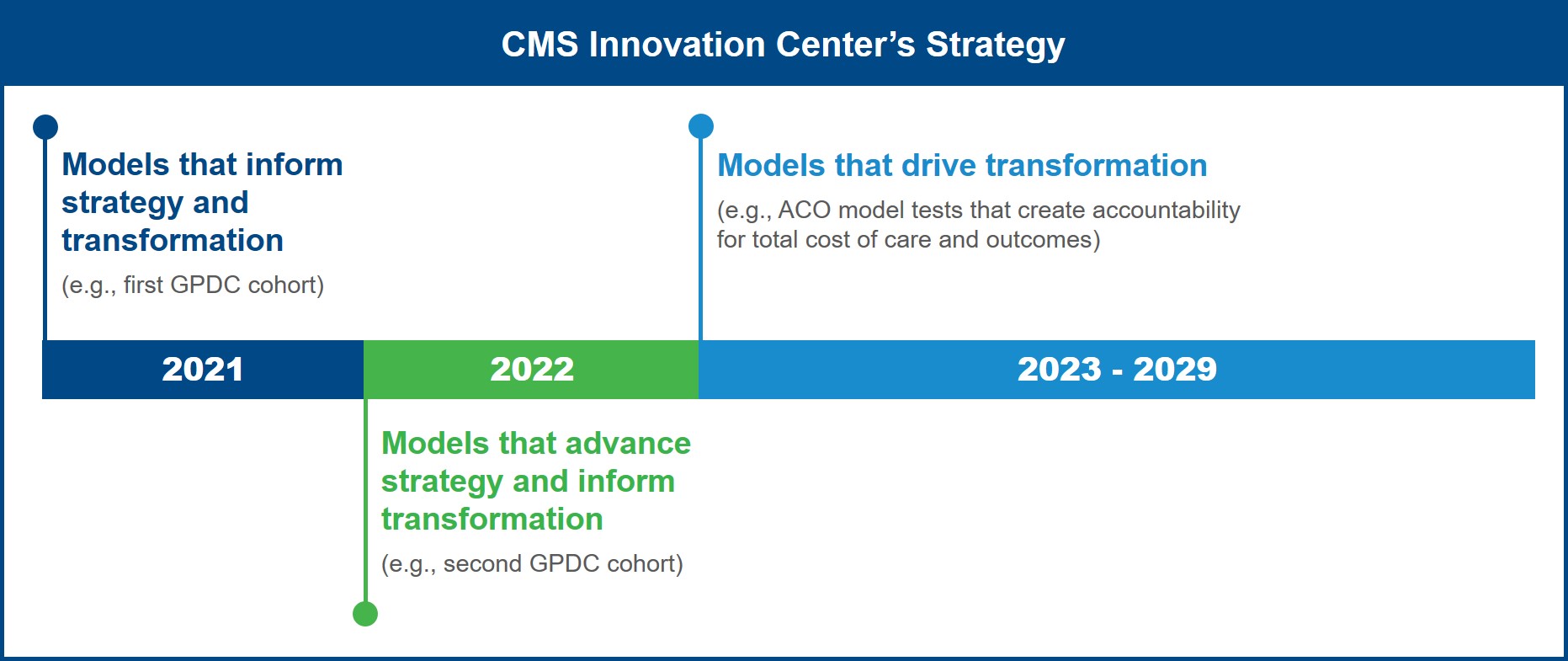
To celebrate more than 10 years of work transitioning the U.S. health system to value-based care, the Center for Medicare and Medicaid Innovation (Innovation Center) is embarking on a strategic initiative to refresh its approach and drive more equitable health outcomes for Medicare and Medicaid beneficiaries. Taking center stage in this effort is a goal for all original Medicare beneficiaries (those in Parts A and B) to be in an accountable care relationship by 2030.
As of January 2021, 22% of original Medicare beneficiaries were in accountable care arrangements while 47% were part of Medicare Advantage plans, with the remaining 31% in traditional fee-for-service (FFS) Medicare. Shifting everyone into accountable care relationships in 10 years is an ambitious goal to be sure. CMS anticipates that this could lead to an additional 30 million beneficiaries (adjusted for growth in the Medicare population) attributed to organizations such as advanced primary care practices, accountable care organizations (ACOs), or similar entities that assume responsibility for care costs and quality.
Note that the Innovation Center’s objective doesn’t necessarily imply that ACOs and other accountable arrangements will look the same as they do today. Starting in 2023, the Innovation Center plans to further refine, test, and evaluate different value-based models, looking to sunset more episodic arrangements and prioritize those that create accountability for total cost of care. This may mean that capitated models, such as the Global and Professional Direct Contracting (GPDC) Model, could become more prominent.As has happened in the past, different models may merge, combining characteristics of current ACO offerings and more advanced total capitation arrangements to form an enhanced approach.
So, what does this mean for providers? For those currently participating in ACOs and other accountable care models, you are on the right track. However, many of these arrangements do not include a mechanism for managing total cost of care. Although your organization may be hesitant to assume this level of risk right now, bear in mind that health care is moving inexorably in this direction, and you may need to adapt to this kind of approach in the not-so-distant future. Starting to think through what that looks like and how you get there is wise.
For those providers that haven’t ventured into accountable care arrangements, you risk being left behind. Not only are Medicare and Medicaid moving in this direction, but commercial models are as well. And these plans may be ahead of CMS in implementing total care capitation, using this approach in some direct-to-employer contracts, ERISA plans, and self-insured arrangements. By embracing accountable care offerings, specifically those that manage total cost of care, providers can remain competitive and financially sound while enabling higher quality, more person-centered care that is more equitable and cost-effective.
To learn more about the Innovation Center’s plans for the future and its strategic refresh, go to https://innovation.cms.gov/strategic-direction-whitepaper.